Thyroid Examinations in Fukushima Prefecture
after the TEPCO Nuclear Accident
目次
- The thyroid examination program in Fukushima Prefecture.
- The high incidence of thyroid cancer in Fukushima Prefecture.
- Is there an association between the level of contamination and thyroid cancer incidence?
- An accurate thyroid cancer case count is essential.
- The decline in thyroid screening rate is a problem.
1. The thyroid examination program in Fukushima Prefecture.
Radioactive iodine contaminated other prefectures as well, but the government limited thyroid examinations to Fukushima Prefecture. In October 2011, Fukushima Prefecture began examining the thyroid glands of children who were 18 or younger at the time of the accident. The planning, implementation, compilation of statistics and analysis of the examinations were all entrusted to Fukushima Medical University. Examinations are carried out every two years until the age of 20, and every five years thereafter using ultrasound equipment.
A flow chart of the patient screening process is shown in the figure below.
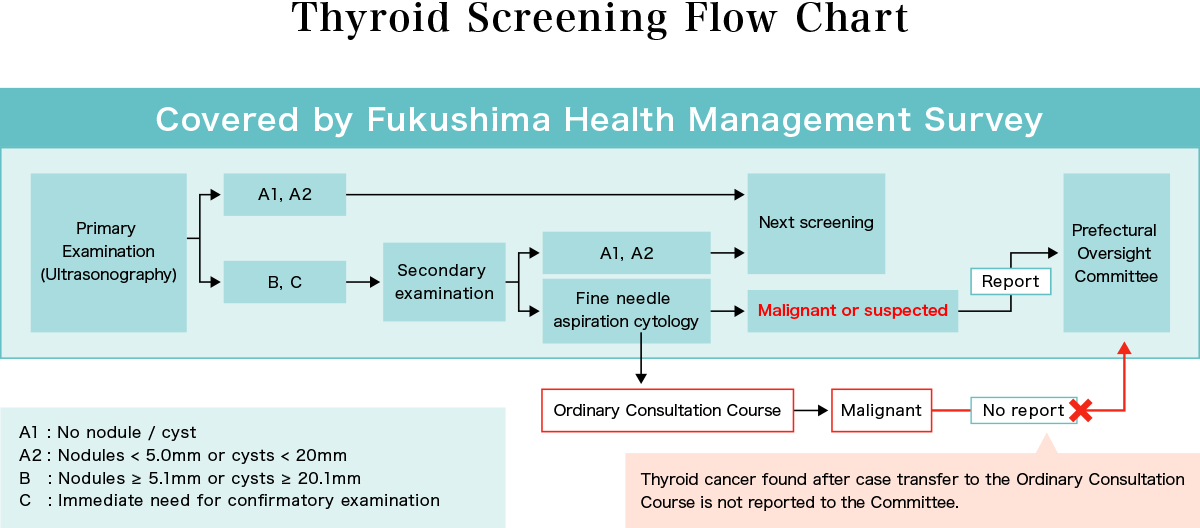
If the primary examination results in an A1 or A2 designation, the next round of testing will be conducted in two years. For B or C results, a second confirmatory examination is recommended, and if deemed necessary, fine-needle aspiration cytology is performed. If the cells are malignant or suspected of being malignant, surgery is performed at the patient’s request, and the final diagnosis of cancer is confirmed based on tissue examination. The number of malignant or suspicious cases confirmed at the secondary examination is reported by Fukushima Medical University to the experts forming the Fukushima Health Management Survey Oversight Committee and made public at the same time.
2. The high incidence of thyroid cancer in Fukushima Prefecture.
The examinations are being conducted on approximately 380,000 children who were 18 and under (including those in utero) at the time of the accident. Currently, the fifth round of screening is underway. The table below shows results up to July, 2023.
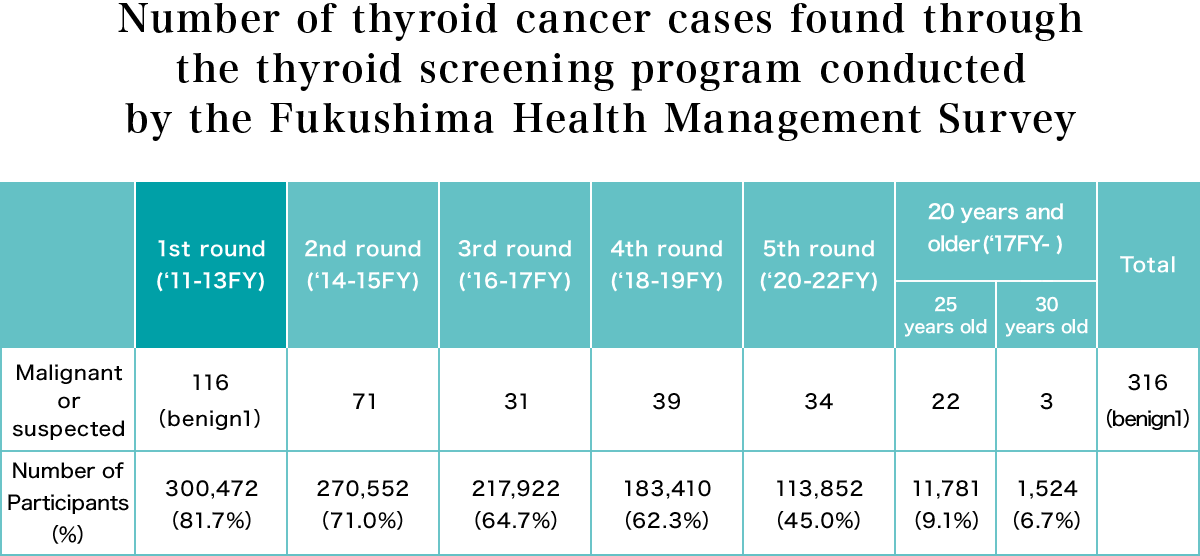
Source: Documents from Fukushima Health Management Survey Oversight Committee (July 20, 2023)
About 300,000 people were examined during the first round, in which 116 cases were diagnosed as malignant or suspected of malignancy, and of the 102 who underwent surgery, one case was benign and 101 were diagnosed as cancer.
The Oversight Committee concluded that “The number of thyroid cancers found is in the order of dozens of times higher than the prevalence estimated from thyroid cancer incidence statistics and other sources.” The Oversight Committee’s interpretation of this situation, however, was that “It has been suggested that we may be diagnosing a number of cancers that would not be clinically diagnosed in the future and that would not lead to death.” This interpretation suggests that the high incidence is either overdiagnosis or a “screening effect.” (In other words, cancers that might have developed naturally in the future were being found earlier than they normally would have because a large number of people were being tested using highly sensitive equipment).
If the first-round result were a screening effect, then the second round should have found no or very few cancers. The second round, however, turned up malignancies or suspected malignancies in 71 patients. 33 of them had been found to have no abnormalities two years earlier. In some cases, the thyroid cancer had grown from an undetectable size to 5.1mm or more during that period. Dr. Shinichi Suzuki, who performs the majority of thyroid operations at the Fukushima Medical University, denies that this is a matter of overdiagnosis because about 78% of the cases involve lymph node metastasis and about 45%, extrathyroidal invasion. Such cases require surgery.
3. Is there an association between the level of contamination and thyroid cancer incidence?
What is the relationship between radioactive contamination and cancer?
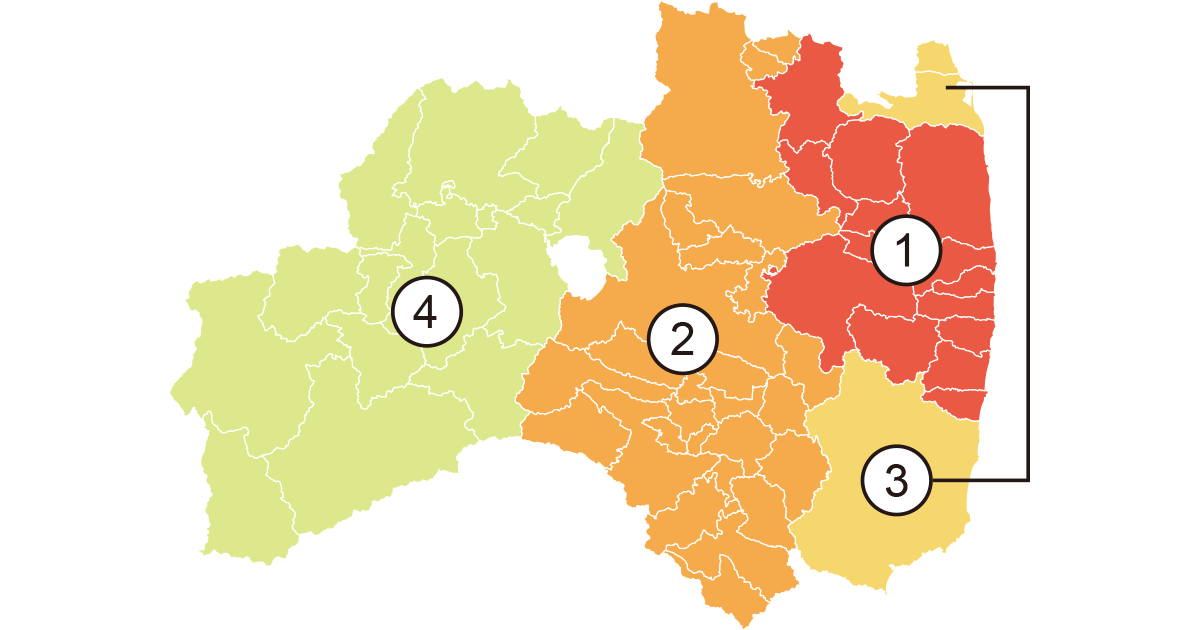
Based on doses measured in March 2011, the Fukushima Prefecture was divided into four areas as shown in the figure above, in the order of descending dose: (1) the evacuation zone (13 municipalities), (2) Nakadori (middle area), (3) Hamadori (coastal area) and (4) the Aizu region (western area).
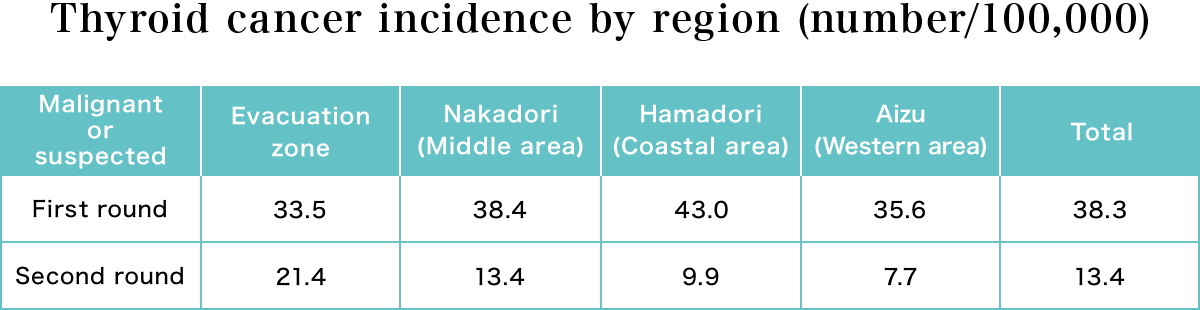
The table above shows the number of cases per 100,000 persons diagnosed as malignant or suspected malignant in each region. Since there was no correlation between the level of contamination and thyroid cancer in the first round of thyroid examinations, the Oversight Committee announced that the high incidence of thyroid cancer was unlikely to be caused by radiation.
In the second round, however, the cancer incidence was highest in the most contaminated evacuation areas and decreased with decreasing levels of contamination. This result is represented by the graph at the bottom of Figure A, which shows the regional thyroid cancer incidence in relation to the contamination level.
After these results were reported, Fukushima Medical University changed the regional classification according to the radiation dose estimated by the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) as shown in Figure B, and re-analyzed the results by dividing the patients into two groups: those aged 6-14 years and those aged 15 years and older, excluding, without explanation, one 5-year-old child.
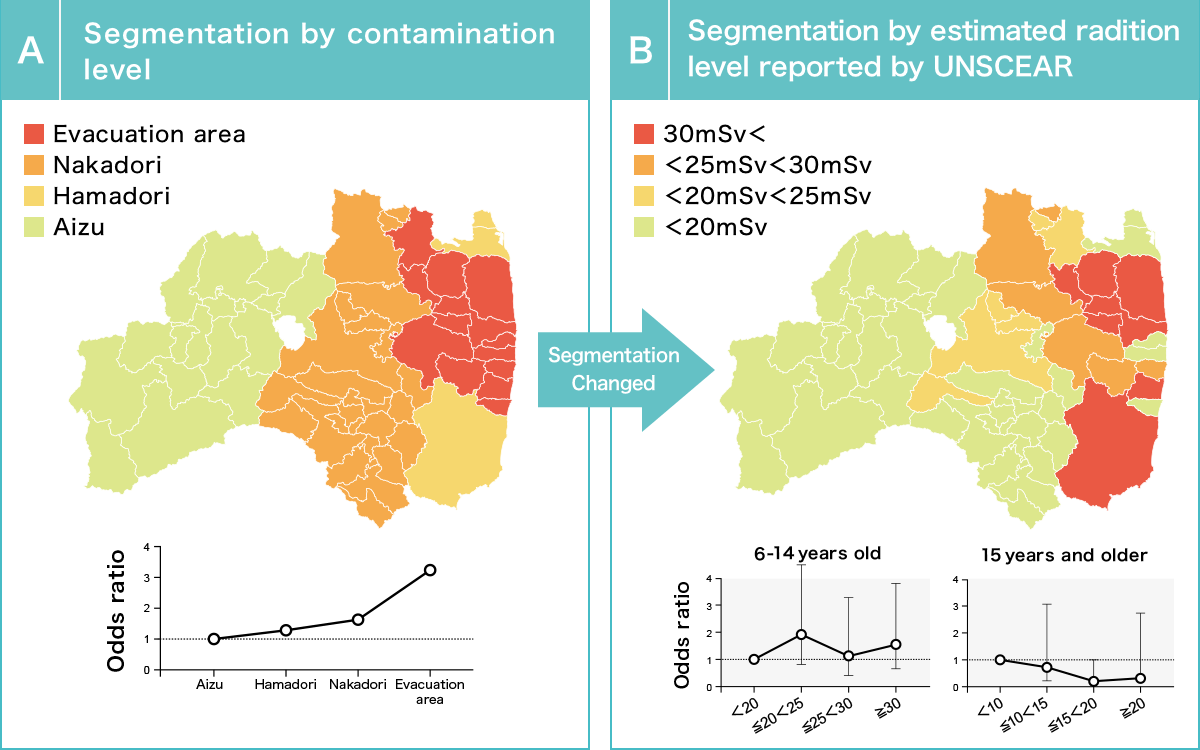
Source: Documents from the 35th Fukushima Prefectural Oversight Committee meeting
As shown in Figure B, in the 6-14 year-old age group, the incidence of thyroid cancer was higher in the 20-25 millisievert area group than in the areas measuring 20 millisieverts and under. At higher doses, there was no dose proportional increase.
On the basis of this result, the Oversight Committee announced that “no association between the thyroid cancers detected and exposure can be recognized,” ignoring the regional differences demonstrated in Figure A. In addition, the result showing that the cancer incidence rate decreases with increasing radiation dose among those over 15 years of age raises questions about the analytical method, but no explanation was provided.
This purportedly scientific study, which ignores regional differences in thyroid cancer incidence rates, re-analyzes data by changing the designation of contaminated areas and introducing a new classification of age groups after positive correlations had been obtained, which moreover neglects to explain some of its own findings, has been severely criticized by experts (Yutaka Hamaoka, Trends in the Science, March 2020, Science Council of Japan; Junichiro Makino, [Kagaku] (Science), August 2019). Neither Fukushima Medical University nor the Oversight Committee has responded to such criticism.
A few members of the Oversight Committee have stated that it is not possible to affirm or deny a causal relationship between the high incidence of thyroid cancer and exposure to radiation at this time.
4. An accurate thyroid cancer case count is essential.
The 3.11 Fund for Children with Thyroid Cancer support project has revealed that there are patients who were not included in the number of thyroid cancer cases announced by the Oversight Committee. If a case is not diagnosed as malignant or suspected of being malignant at the secondary examination, the patient is transferred for follow-up in the “Ordinary Consultation Course,” or referred to regular medical care (Thyroid Screening Flow Chart). It was found that patients who were diagnosed with cancer during this follow-up period and underwent surgery were not reported to the Oversight Committee. Without knowing how many of the follow-up patients developed thyroid cancer, there is no meaningful way to analyze the relationship between cancer and radiation exposure.
In response to this criticism, the Fukushima Medical University announced 19 additional cases (as of March 2020), but these consisted only of patients who had been operated on at Fukushima Medical University. In addition to these 19 patients, the 3.11 Fund is aware of more than 15 additional patients who were operated on at other hospitals. These cases were not included in the investigation of a possible causal relationship. There may be other patients who have not yet been identified.
Is it possible to analyze this crucial relationship on the basis of such an incomplete record and to conclude that high incidence is “not recognized as an effect of radiation”? Shouldn’t experts at Fukushima Medical University, the Oversight Committee, Fukushima Prefecture, and the Ministry of the Environment strive to come up with conclusions based on accurate patient numbers and doses in order to regain the public’s faith in science?
5. The decline in thyroid screening rate is a problem.
The percentage of people who get thyroid examinations has been declining through the successive rounds of screening.
Moreover, although only 8.4% of those over the age of 20 have been screened, 7 have been found to have thyroid cancer. It has been reported that if a nodule is diagnosed after it has grown unnoticed, the area to be removed becomes larger and the rate of distant metastasis is increased. In principle, early detection and early treatment are the key to cancer treatment. Particularly in Fukushima Prefecture, where many people were exposed to radiation released by the nuclear accident, regular examinations are important for early cancer detection. Examinations can be done without risk as screening is performed using ultrasonography, not radiation.
One of the reasons for the decline in the screening rate is that an increasing number of high school graduates have moved out of the prefecture, making it harder for them to get tested. In addition, some members of the Oversight Committee have emphasized the disadvantages of overdiagnosis, while others have argued that examination of students at school interferes with their studies.
No convincing evidence has been presented to support the conclusion of overdiagnosis, and Dr. Suzuki, who has performed the majority of thyroid surgeries at the Fukushima Medical University, as well as other physicians, disagree that overdiagnosis is the issue.
In a survey of recipients conducted by the Fund in 2021, nearly 90 percent of them responded that they were glad their cancer was found at an early stage and wanted the screening program to be continued.
We hope that the Fukushima Prefectural Government will listen to the people of the prefecture, understand the causes of the decline in the screening rate, and work to improve it.
In addition, if you are reading this and are eligible for a thyroid exam, please don’t hesitate to get tested!
Created: March 2021, Last updated: July 2023
-
Dose Dependency and the Mechanism of Carcinogenesis
-
The Nuclear Power Plant Accident and Thyroid Cancer
- Why did people worry about thyroid cancer after the Fukushima Nuclear Power Plant Accident?
- Why should people take iodine tablets (“stable iodine,” “potassium iodide”) in the event of a nuclear accident?
- When should iodine tablets be taken? What is the required dosage?
- Did the people of Fukushima Prefecture take iodine tablets?
-
Thyroid Examinations in Fukushima Prefecture after the TEPCO Nuclear Accident
- The thyroid examination system in Fukushima Prefecture.
- The high incidence of thyroid cancer in Fukushima Prefecture.
- Is there an association between the level of contamination and thyroid cancer incidence?
- An accurate thyroid cancer case count is essential.
- The decline in thyroid screening rate is a problem.
-
What Can We Do to Protect Children’s Health?